
A full list
You have no items in your basket
Psoriasis is a long-term (chronic) scaling disease of the skin, which affects around 1 in 50 people, about 1.3 million, which is around 2% of the UK population. It appears as red, raised scaly patches known as plaques. Any part of the skin surface may be involved but the plaques most commonly appear on the elbows, knees and scalp. It can be itchy but is not usually painful. Nail changes are present in nearly half (40-50%) of people and some people can develop psoriatic arthritis.
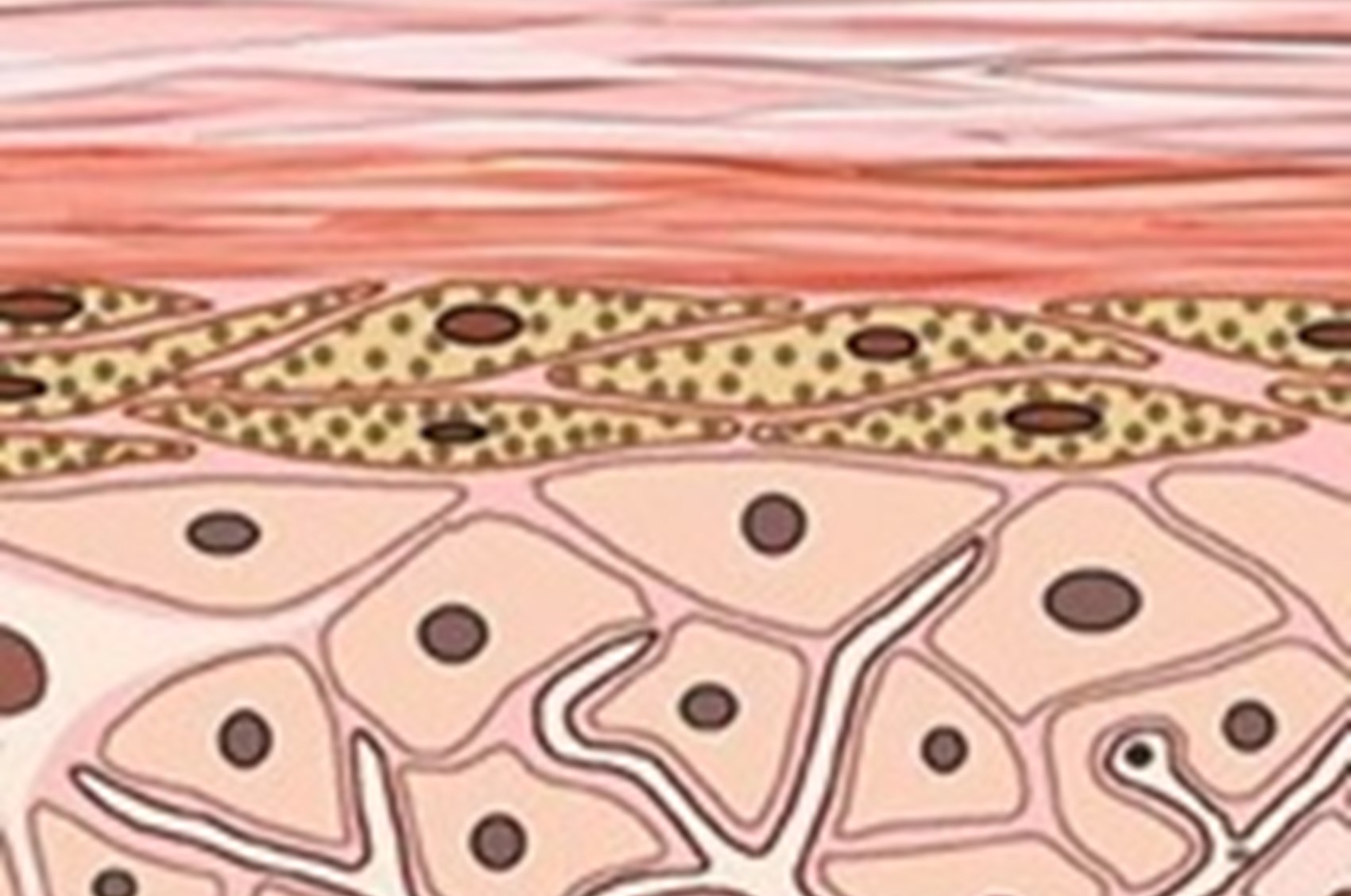
Normally a skin cell matures in 21 – 28 days and during this time it travels to the surface, where it is lost in a constant invisible shedding of dead cells. In patches of psoriasis the turnover of skin cells is much faster, around 4 – 7 days, and this means that even live cells can reach the surface and accumulate with the dead cells.
This process is the same wherever it occurs on the body.
Psoriasis is not contagious.
Remember, although psoriasis is a chronic long term condition with no cure it can be controlled and go into remission (go away). Not all people will be affected in the same way and doctors will class the condition as mild, moderate or severe.
Mild psoriasis which affects around 1 million people in the UK or 4 out of 5 (80%) is where there are a few patches that may need treatment but are not likely to cause problems and can be easily controlled.
Moderate psoriasis which affects around 200,000 people in the UK, which is about 3 out of 20 (15%) is where more skin is involved and the condition widespread but again can usually be controlled with self-management under GP or nurse supervision.
Severe psoriasis which affects about 65,000 people in the UK or 1 out of 20 (5%) is where large areas are covered with psoriasis and the condition is becoming difficult to self-manage or is no longer responding to treatment. At this stage referral to secondary care at a local hospital out-patient department or in extreme cases an in-patient stay may be felt necessary in order to provide optimum care and monitoring.
Around 1 in 3 (30%) of people with psoriasis may develop an associated psoriatic arthritis also known as psoriatic arthropathy, which causes pain and swelling of the joints and connective tissue, accompanied by stiffness, particularly in the mornings. Most commonly affected joints are the hands, feet, lower back, neck and knees, with movement in these areas becoming severely limited. Chronic fatigue is a common complaint linked with this condition. If you are experiencing mild aches and pains and have psoriasis, albeit very mildly, consult your dermatologist for further advice and if necessary a referral on to a rheumatologist for further assessments will be made.
The exact cause of psoriasis is unknown, although it is known that your genetic make up plays a significant part. It is also known that psoriasis is the result of something going wrong with the immune system, which can be set off by certain trigger factors.
Normally, the outer layer of dead cells, which form the surface of our skin, get rubbed off or fall away as new cells are made to replace them. This turnover of skin cells happens without us being aware of it over a period of around 28-days. In psoriasis, the production of new cells occurs too quickly. Skin cells divide and push to the surface in around 4 - 7 days. As a result, excessive numbers of live cells reach the surface before they have matured and build up to form raised, red patches. These patches are usually covered with dead cells to form the fine, silvery scales or thick white plaques that are so characteristic of psoriasis.
It affects men, women and children alike. It can appear at any age in varying degrees but usually between the ages of 10 and 30. The extent of disease varies enormously from a minute patch to large patches covering most body areas. Psoriasis can also run in families and much research is being done into the genetics of this disease. It is known that the disease is multi genetic and therefore children may not necessarily inherit psoriasis.
If both parents have psoriasis then the risk of children developing psoriasis is 15 out of 20 (75%) and if one parent has psoriasis, the risk of children developing the disease is 3 out of 20 (15%). If a brother or sister (but neither parent) has psoriasis then the risk of other siblings developing psoriasis is 1 out of 5 (20%). Therefore, if you have psoriasis, your children will not necessarily develop it.
Genetic predisposition means an inherited tendency to develop the disease. Recent research has greatly increased our knowledge about how and what we inherit from our parents and the role played by genes. As our knowledge increases so does our appreciation of the complexity of the process. While it was originally hoped that a specific disease might be associated with a specific gene, it now appears that for many diseases that have a genetic component, including psoriasis, there are probably multiple genes involved in producing the sequence of events that results in the expression of disease. This is further complicated by the way these genes interact.
However, the evidence to support the belief that a genetic predisposition plays a major role in the cause of psoriasis can be summarised as follows:
There is a higher than expected frequency of certain characteristics of blood cells in people with psoriasis and their close relatives. However, some people with psoriasis have no family history at all.
It is important to understand that genetic predisposition does not mean a 100 percent guarantee that the disease will appear. Other initiating or trigger factors may act together with genetic predisposition to set the disease process in motion.
Your immune system is designed to protect you against infection and disease. It is made up of a number of white blood cells (T cells) that patrol the body in search of cells and proteins that should not be there. All your own cells have special identity tags to help your immune system recognise them. Sometimes, however, the immune system over-reacts or even attacks parts of the body to cause problems.
In psoriasis, T cells are put into action by mistake and become so active that they trigger other immune responses, which lead to inflammation and to the rapid turnover of cells which pile up on the surface of the skin, forming raised red scaly plaques. This inflammation can also affect the joints causing psoriatic arthritis.
The exact mechanism that stimulates these T cells into their harmful behaviour is not known but a number of trigger factors have been discovered.
Although the underlying cause of psoriasis stems from your body's immune system, the trigger factors that can make it worse or cause flare-ups include:
The bottom line is that the lack of precise information on the cause of psoriasis severely hampers the search for a cure. However, the current state of information has resulted in the development of new effective treatments, all based on trying to correct the faults within the immune system. It is hoped that future more effective treatments will be developed as understanding of the complex problems within the immune system increases.
Meantime, more straightforward actions such as reducing alcohol intake, stopping smoking and trying to cope with stress can be recommended. The course of psoriasis is unpredictable. Whilst remission of symptoms can occur, it may take weeks, months or even years.
It is widely accepted that psoriasis can severely affect an individual’s quality of life although for many the condition is mild and a mere inconvenience. The severity of the disease does not always relate to the severity of anxiety that an individual will have. The area where the psoriasis is located such as the hands or face can severely affect an individual’s ability to work or lead to discrimination due to ignorance.
Loss of confidence and self-esteem can make you feel unattractive and have a negative effect on your relationships. You may even feel a sense of mourning for not being able to do the things you once did such as wearing shorts, sunbathing, swimming or even just going out. Unfortunately, the more you worry about your skin, the worse you will feel. Although stress does not cause psoriasis, it can trigger a flare-up.
Remember that psoriasis is common and affects as many as 1 in 50 people
There may not be a cure yet but there is much you can do to help maintain and control your psoriasis. Your general practitioner/dermatologist will be best placed to keep you informed of all new treatments around and to advise you on the best treatment programme for you.
Remember. Your treatment can only be as good as you allow it to be - that means if the treatment takes six weeks, you have to do it as instructed for six weeks and no ducking out!
Finding out all you can about psoriasis and having a full working understanding of it can be very helpful in coping with the problem. Look out for any emerging patterns, stress levels and any event that may trigger flare-ups.
A healthy diet is important for well-being and can reduce your risk of many long term illnesses, including coronary heart disease, inflammatory conditions and even cancer. However there is no clear link between what you eat and the severity of psoriasis symptoms.
There are a lot of dietary supplements available over the counter and available on line. Please remember that some of these products may not be of a high quality or reputable standard. Please always consult your doctor or healthcare professional before embarking on any supplementation to avoid overdosing in vitamin nutrients as these may cause undesired side effects.
Again there are numerous products on the market and these should be used with caution and under strict supervision of your doctor or healthcare professional as these too, taken in combination with any other medications may have adverse side effects causing unnecessary discomfort. One in particular is St John's Wort which can in some cases cause increased sensitivity to light which can or may cause problems for some people undergoing phototherapy (light treatment) for their psoriasis. Always advise your doctor or healthcare professional on any herbal or dietary supplements that you are taking or may wish to take as this may be a factor in future prescribing for your condition.
There is a huge variety of vitamin supplementation available for purchase. Again, as with herbal and dietary supplements, before embarking on such supplementation you should discuss it with your doctor or healthcare professional. If you have adequate vitamin nutrition in your diet, taking supplementary vitamins or indeed taking larger doses of them than recommended may cause more harm than good. In some cases toxicity can occur.
There are a variety of alternative approaches that can be undertaken alone or in combination with conventional therapies. It is essential if you are considering any alternative approaches to please discuss this with your doctor or healthcare professional as they may be detrimental to your health.
Such alternative approaches could entail Chinese Medicine, Acupuncture, Magnatherapy, Ayurvedic Medicine, Aromatherapy, Homeopathic Medicine, Yoga, Spa Treatments, Shiatsu, and Naturopathy. It is always advisable to fully research and find a reputable qualified practitioner who follows correct protocols for their clients. There are organisations that may be useful to contact for further details and advice. With this information you and your doctor or healthcare professional will be better placed to discuss what is best for you.
If you think you have psoriasis, go and see your GP. Don’t forget, if you are also experiencing aches and pains in any of your joints (psoriatic arthritis), have any other symptoms including nail or scalp involvement or if you have a family history of psoriasis, inform the doctor. This will assist with diagnosis and treatment.
The doctor may decide to start treatment themselves or refer you to a dermatologist (skin specialist doctor) for advice. It is essential to seek medical advice because of confusion in diagnosis. Although many treatments are available over the counter (OTC) from pharmacies your doctor may be able to prescribe particular treatments that are specifically for psoriasis.
If you are referred for further treatment or advice it is likely to be to outpatients at your local hospital where a consultant dermatologist or a specialist dermatology nurse will assess you or it may be to another General Practitioner (GP) with enhanced role (GPwER) often referred to as GP with special interest (GPwSI).
It is likely that you may be offered the same treatment that your GP has already given you or other treatments that your GP is unable to prescribe.
Unfortunately, not at the moment. Much research is being done and in the last decade great strides have been made in understanding what goes wrong in psoriasis, so there is good cause for optimism. In the meantime there are a number of treatments that are effective in keeping the problem under control. The art of treating psoriasis is finding the best form of treatment for each individual. There is no single solution that is right for everyone.
Psoriasis has a fascinating story, from ancient times, through to the modern scientific breakthroughs. Read more.